Fear of Health Facilities and Ebola Treatment Units
Key Considerations
Fear of health facilities and ETUs can lead to hiding Ebola victims and/or having them treated at home by untrained workers. These untrained workers can be individuals that the victims would normally turn to for help, such as traditional healers, and off-duty health facility workers (sometimes anyone who works for a health center is consulted, even if that person is in maintenance). Often, they will not wear protective clothing.
When addressing the avoidance of ETUs and health facilities, consider the following:
Collaborate with health systems strengthening teams and agencies that work in MNCH, HIV/AIDS or other health areas to promote safe usage of health facilities.
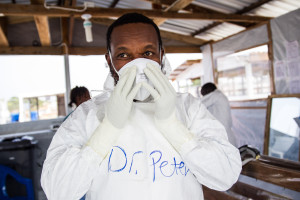
Address communities before ETUs are built and hold dialogues with community members; ensure that communities understand what the ETUs are and what they do, and why HWs wear PPEs; and make sure that community members have a role.
Always communicate clear steps that community members can take when they or someone they know is ill, such as informing a community leader, calling a hotline, etc.
Important people to involve in your communication efforts
Ebola survivors, HWs, CHWs and volunteers, Ebola task forces, district health teams, local champions, community leaders, mass media
|
Common Causes/ Contributing Factors |
Sample Message Response |
Sample Activities and Implementation |
|
High death rates and lack of trust in foreign- or government-led facilities
Lack of respect or information to communities and the family of victims
Misunderstandings/lack of information about incoming ETUs and PPEs in communities, and lack of community buy-in
Misunderstandings about survival rates; lack of information of whether health centers are safe places to go when sick
All of these contribute to the perception that ETUs are places where people go to die and health facilities are places where you can catch Ebola |
Consider messages that reflect how we are “in this together,” giving the community the real sense they have a role to play in ending Ebola. They could include messages about what to do or where to go when sick with an illness that is not Ebola, and the benefits of doing so. Governments and agencies need to work with community leaders and other members to communicate about incoming ETUs and PPEs to communities so they do not inflame panic.
Messages need to focus on how early treatment can increase the chances of survival. Some examples include:
Remember, if anyone is sick, call XXX (or see X) so they can advise you on the best health services and send the help you need.
While you can’t visit your sick friend/family member in the isolation part of the center (red zone), you will be called for you to know how he/she doing OR you can still go to the center and discuss with the staff who take care of him/her
|
Radio dramas and radio discussions with HWs and trusted leaders who dispel rumors and explain the purpose of the ETUs, HWs wearing PPEs and the safety of health facilities
Promote information on what to do when sick with something other than Ebola and provide clear benefits in mass media, with stories of community members who have been treated
Create community-level activities that promote dialogues about visiting ETUs or health facilities, prompting discussion and reflection; incorporate survivor stories
Ensure community ownership of ETUs and other treatment or health facilities; hold dialogues with communities to get their input and communicate agreed-upon safe burial practices back to the community
Promote stories about survivors and others who are stigmatized (e.g., HWs, burial teams) through mass media, videos and community events
Try to organize visits for communities or families to ETUs to help demystify them. Alternatively, create short videos of the ETUs and show them to alleviate fears
Provide a bridge between the patient and his/her family and community—this might include establishing a cadre of community health volunteers who can guide community members to services when they are ill and interface with staff and the family for patient visits or calls |