Appendix C: Breastfeeding Situation Analysis (Questions to Answer)
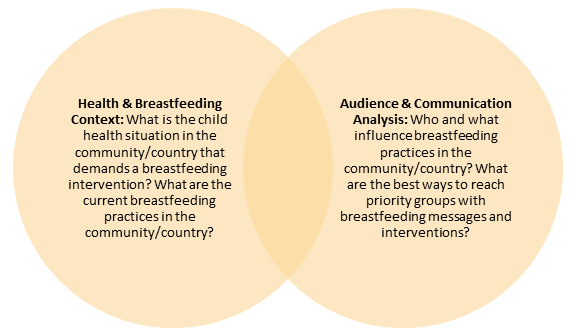
REMEMBER: The situation analysis has two main sections, Health and Breastfeeding Context and Audience and Communication Analysis, and it should help you answer five big questions:
- What is the child health situation in the community/country that demands a breastfeeding intervention?
- What are the current breastfeeding practices in the community/country?
- Where, with whom, and to what extent do they need to be changed?
- Who and what influence breastfeeding practices in the community/country?
- What are the best ways to reach priority groups with breastfeeding messages and interventions? FBOs in particular will want to be sure to identify faith-related assets they can use to help people change breastfeeding practices. These might include religious texts and teachings, religious groups and leaders, groups within religious institutions such as youth groups, women’s groups, men’s groups, religious broadcasts, and other available assets.
The types of questions you need to ask for each section are detailed below. While each list is fairly comprehensive, you might choose to address more, different or fewer questions.
Health Context
These health questions help you understand how strong the need is for breastfeeding SBCC intervention:
- What are the neonatal and child mortality rates in the country?
- What are the stunting and wasting rates in the country?
- What percentage of children suffer from childhood illnesses such as diarrhea, pneumonia and other respiratory illnesses, malaria, and ear infections?
Even though optimal breastfeeding is better for almost all children and families, if child malnutrition, illness, and mortality are not common in your country/community, you might decide to use your human, technical, and financial resources to address a different problem.
Breastfeeding Context
If you decide to work to improve breastfeeding practices, the answers to these breastfeeding questions will help you understand current infant and young child feeding practices in your community/country (and, to some extent, who influences them).
- What proportion of women exclusively breastfeed for the first six months? Initiate breastfeeding within the first hour? Continue to breastfeed and add complementary feeding from 6 to 24 months of age?
- How many times/meals per day do breastfeeding mothers eat? How much do they eat at each meal? How many types of foods do they eat each day? Do they include leafy greens, orange fruits/vegetables and animal proteins (e.g., eggs, fish)?
- Do mothers give the baby the yellowish substance (colostrum) that first comes from the breast?
- Do mothers breastfeed the newborn within the first hour after birth? Why or why not?
- Do mothers wait hours or days to breastfeed? If so, how many? Why?
- Does anyone give the baby another liquid or food before they ever give breast milk? What are the reasons for this practice (traditional, cultural, religious, other)?
- How many times a day do mothers breastfeed babies between birth and 6 months of age?
- Are boys and girls fed differently within the first six months? From age six months to 24 months? If so, what are the differences? Why are they fed differently?
- Are infants ever given water, tea, or other liquids or foods in between feedings within the first six months? Starting at what age? Why?
- Are infants breastfed on a schedule, or do they breastfeed whenever they are hungry? Until what age? Why?
- Do women ever express milk to give the baby later? If so, how, where, and for how long do they store the milk?
- What is used to give the baby expressed milk? A bottle with a nipple/teat? A spoon? A cup? Something else? Why?
Answers to these questions will help you understand how some typically important factors impact breastfeeding practices in your community/country and how to prioritize audiences/groups. You might find other factors important.
- In what ways do husbands or other family members (e.g., grandmothers) support women who are breastfeeding?
- How available is infant formula? How affordable is it to low-, middle-, and high-income mothers?
- Is there a tradition of giving infant formula or other breast milk substitutes?
- Can the costs of sub-optimal breastfeeding practices (such as formula, cow’s milk, medical visits, medicines) be estimated? What are they? Do such costs matter to mothers, fathers, or other family members? Why or why not?
- What opportunities exist to increase the proportion of children whose mothers follow optimal breastfeeding practices?
- How have breastfeeding practices/patterns changed over the past 5-10 years (more or less exclusive breastfeeding, for longer or shorter period, changes in continuing to breastfeed while providing complementary feeding, changes in maternal nutrition)?
- What audiences/priority groups know and think about infant and young child feeding
- What the social norms are regarding breastfeeding
- How policies affect breastfeeding practices
- What happens in health, religious, and other facilities to encourage or discourage optimal breastfeeding practices
- What are the best ways to reach your audiences/priority groups
Knowledge and Attitudes
Answers to these questions will give you a good idea of what your audiences/priority groups know and think and do about breastfeeding. Exploring them deeply can also help you understand why they believe or feel the way they do about various aspects of infant and young child feeding.
- What percentage of providers, women, men and other influential stakeholders have accurate knowledge about optimal breastfeeding practices?
- What do the various cadres of health care providers–including ANC providers, SBAs, TBAs, CHWs, and health promoters–know about breastfeeding advantages? What do they know about the risks of not following optimal breastfeeding practices?
- Are there common misconceptions or misinformation about colostrum and other aspects of breastfeeding?
- What do women, their partners, and other gatekeepers perceive as the benefits of optimal nutrition for lactating women?
- What do women, their partners, and other gatekeepers perceive as the benefits of breastfeeding in general, early initiation, exclusive breastfeeding, and complementary feeding?
- What do women, their partners, and other gatekeepers perceive as barriers to early and exclusive breastfeeding, and breastfeeding while providing complementary feeding?
- What do women, their partners, and other gatekeepers perceive as making optimal breastfeeding practices easier?
- What do women, their partners and other gatekeepers perceive as the benefits of giving under six-month-olds infant formula and other foods and liquids?
- What do women, their partners, and other gatekeepers perceive as risks associated with sub-optimal breastfeeding practices?
- What do women, their partners, and other gatekeepers perceive as the barriers to optimal nutrition for lactating women?
- How do providers perceive early and exclusive breastfeeding, mixed feeding, breastfeeding while providing complementary feeding, and artificial feeding (formula feeding)?
- How do use and perceptions of artificial feeding impact breastfeeding perceptions and practices?
Normative and Structural Considerations
These questions explore social norms.
- What are the gender norms in country among couples, both married and unmarried, and how do these affect optimal breastfeeding practices?
- Who in the family decides how infants and children under 2 are fed? Who influences these decisions?
- Who are the stakeholders, key players, and gatekeepers who impact or influence breastfeeding practices?
- How are these stakeholders, key players, and gatekeepers impacting or influencing breastfeeding practices?
- Do mothers of newborns/infants follow a restricted diet? If so, to what extent does this diet provide adequate nutrition for a nursing mother?
- Under what circumstances is it acceptable to breastfeed? Under what circumstances is it not acceptable? Are there any taboos around breastfeeding? If so, what is their purpose?
- How common is it for women to breastfeed in public?
- How does the level of income affect breastfeeding practices? Do poorer women and couples have access to accurate information about breastfeeding? Do they have particular pressures or challenges that impact breastfeeding practices?
- How does education level affect breastfeeding practices?
- What proportion of women/new mothers work outside the home?
- How do the workload responsibilities of mothers, either in or outside the home, impact breastfeeding practices?
These questions address policies and programs that might impact breastfeeding practices.
- Are there policies in place to encourage and enable working women to continue breastfeeding? Are these policies well known? How often are they followed? Are they enforced?
- What government programs exist to encourage optimal breastfeeding practices?
- What government programs exist to improve nutrition?
- What regulations or policies govern supply, distribution, and availability of infant formula? How might these affect breastfeeding practices?
- What resources are in place to support optimal breastfeeding practices?
- What existing channels (e.g., national health worker volunteer program) can be leveraged for reaching women, partners, gatekeepers, and providers with information about optimal breastfeeding practices?
These questions explore faith-based assets and norms.
- What kinds of programs have FBOs, or religious institutions (including yours) carried out to improve the health, nutrition, and survival of mothers or children?
- What other groups/organizations have mounted programs in your community related to breastfeeding, maternal-child health, or nutrition? Is there a way to learn from what they did/do? Who can give you information and good advice?
- Does your FBO/religious institution have women’s or men’s groups that do or could promote breastfeeding? Can they promote breastfeeding in the broader community?
- Does your FBO/religious institution have groups that do or could provide support to women who have trouble breastfeeding?
- What do your religious texts or teachings say that supports breastfeeding?
- What do your religious texts or teachings say that could discourage breastfeeding in public or in private?
- To what extent is culture or religion a factor in breastfeeding practices and care-seeking for women, infants and children?
- How comfortable is your constituency/congregation with talking, hearing about or seeing breastfeeding?
Service Provision
These questions explore whether and how ANC might impact breastfeeding practices.
- What percentage of pregnant women seek antenatal care? How often?
- How early in the pregnancy do women seek antenatal care?
- How and how often is breastfeeding addressed during antenatal care?
- Are women/couples encouraged to make a decision about breastfeeding before the child is born?
- Do ANC counseling guidelines ensure adequate information on breastfeeding, including benefits, risks of not breastfeeding, when and how often to breastfeed?
- Do ANC providers have adequate skills to counsel and problem-solve to support the decision to exclusively breastfeed from birth to six months?
These questions explore the role of various types of providers in breastfeeding practices.
- What percentage of women deliver with a skilled birth attendant (SBA) [1]? With a traditional birth attendant (TBA)? Alone or with an unskilled family member?
- What level of provider (doctor, nurse, midwife etc.) normally provides breastfeeding and nutrition advice and support?
- To what extent do community health workers (CHWs), TBAs, and other community-based health personnel provide breastfeeding and nutrition advice and support?
- Does advice from the different types of providers differ? If so, why and in what way?
- Do counseling guidelines ensure adequate information on breastfeeding, including benefits, risks of not breastfeeding, when and how often to breastfeed and problem-solving?
- Do ANC providers have adequate skills to counsel and support optimal breastfeeding?
- Are health workers providing appropriate consultation on optimal breastfeeding?
- What are the costs of services associated with breastfeeding counseling and follow-up?
These questions explore how health systems and health facilities might or do impact breastfeeding practices.
- Do the health facilities in your area participate in or adhere to the recommendations of the Baby-Friendly Hospital Initiative?
- Are delivery wards and post-delivery practices conducive to early initiation of breastfeeding?
- Is infant formula available at health centers? If so, to whom? For what reasons is it given?
- Do the health facilities in your area have and follow a written breastfeeding/IYCF policy?
- To what extent are breastfeeding guidelines up-to-date, disseminated, and followed?
- Are post partum services for women and newborns provided and their use encouraged?
- What other structural or health system barriers affect optimal breastfeeding practices?
Media and Communication
- Do couples communicate about breastfeeding or other child health/feeding practices? What about other family or community members such as grandmothers or peers?
- Through what channels do FBOs and religious institutions most effectively communicate with their members?
- Through what channels (including media and interpersonal) do providers, women, and their partners prefer to receive health-related information?
- What communication materials and programs already exist related to breastfeeding and IYCF?
- What channels can support the level of communication needed to increase knowledge and practice of optimal breastfeeding?
- What is the technical and organizational capacity of media partners?
- What are the characteristics of the people who access national and regional radio/TV stations?
- Are any national or regional radio/TV stations currently broadcasting information or shows about optimal breastfeeding (or have they recently broadcast relevant information)?
- Are any national or regional radio/TV stations currently broadcasting information or shows dealing with nutrition or maternal, newborn and child health?