What is SBCC?
SBCC is an approach that promotes and facilitates changes in knowledge, attitudes, norms and beliefs, and promotes desired healthy and safe Ebola behaviors and practices. SBCC also supports broader social change to improve health systems and health outcomes through political dialogue, collective action and individual behavior.
Community resistance is one of the biggest obstacles to stopping Ebola. As such, SBCC is an essential component of the Ebola response to contain the disease. Using SBCC approaches, such as social mobilization and mass media to engage communities, helped facilitate individuals and communities to change their behaviors in ways that helped contain outbreaks in the past.
Simply defined, SBCC uses the most powerful and fundamental human interaction—communication—to positively influence social dimensions of health and wellbeing.
A strategic SBCC approach follows a systematic process to analyze a problem in order to define key barriers and motivators to change, create a strategy, and then design and implement a comprehensive set of interventions to support and encourage positive behaviors.
A communication strategy provides the guiding design for SBCC Ebola campaigns and interventions. Developing a strategy involves setting communication objectives, identifying intended audiences, and determining consistent messages for all materials and activities. This process includes identifying which communication channels can best reach the intended audiences. Channels include mass media, information and communication technology (ICT), participatory communication engagement approaches, and interpersonal counseling and communication (IPC/C) for service providers, among others.
In short, strategic SBCC is:
Science-based
Client-centered
Participatory
Benefit-oriented
Service-linked
Multi-channeled
Technically high quality
Advocacy-related
Scaleable
Sustainable
Results-oriented
Cost effective
One of these models is the “P Process” (right), which provides a step-by-step roadmap to guide the user from a loosely defined concept about changing behavior to a strategic and participatory program that is grounded in theory and has measurable impact.
The P Process has five steps:
Step 1: Inquire
Step 2: Design the strategy
Step 3: Create and test
Step 4: Mobilize and monitor
Step 5: Evaluate and evolve
Three cross-cutting concepts are embedded in the P Process, which, when integrated into the strategic process, ensure that SBCC approaches are most effective:
SBCC theory
Stakeholder participation
Continuous capacity strengthening
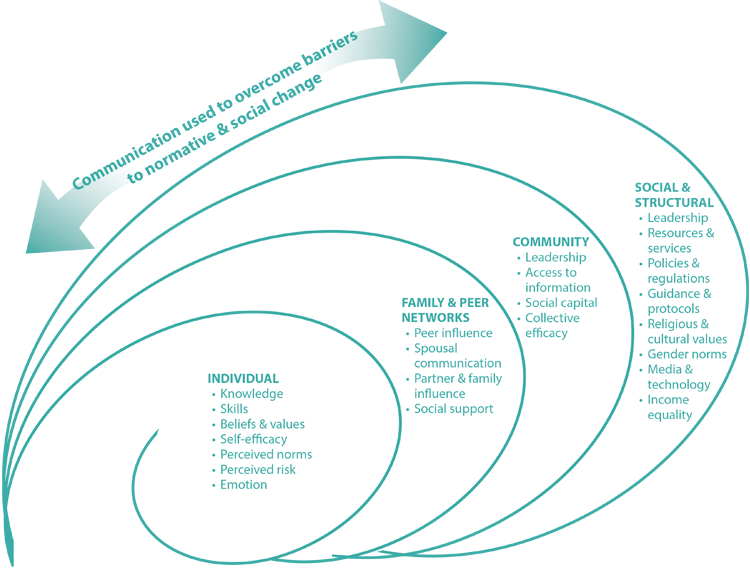
Many factors influence a person’s behavior at the individual level, and beyond it to the family, community and social/structural levels. The Socio-Ecological Framework summarizes the levels of influence on behavior. As the framework illustrates, behavior change can happen through activities that target those four levels.
Take the example of a family living in an urban environment at risk of an Ebola outbreak. The program wants to help families avoid Ebola should there be an outbreak. Consider all of the factors at each level of the Socio-Ecological Framework that can influence these families’ abilities to make healthy decisions.
At the family level, each individual needs information and skills related to knowing: what Ebola is, how it is transmitted, what their risks are, how to respond when someone shows symptoms, how to practice safe burials, and how to get more information and treatment. In addition, families need to learn to embrace survivors and welcome them back into their homes and the community.
At the community level, leaders need to be mobilized and trained to provide proper guidance to community members and ensure acceptance without discrimination.
Setting up feedback loops between community members and services will provide vital information to service providers on community perceptions of services, and cultural and social practices. These mechanisms will better ensure that services are tailored to community needs and encourage health-seeking behaviors among community members.
At the social/structural level, systems should allow for quick containment of Ebola should an outbreak occur. This might include well-supplied treatment facilities, coordinating mechanisms, hotlines and volunteer training. It might also involve bylaws and policies that support containment. Supportive norms and policies around Ebola survivorship and treatment seeking will allow people to get information and access services with confidence.
At each level, there are factors that affect behavior in a positive way, called facilitators, and factors that affect behavior in a negative way, called barriers. Examples of barriers include treatment centers without adequate supplies, slow or poor quality service delivery, and condescending service providers that can influence individual, family and community behavior about trusting and using health care services. The facilitators and barriers in the Ebola context are described in more detail in Chapter 6, and within the Appendixes are the Illustrative Ebola Communication Strategy (Appendix A) and the Ebola Communication Response Tables (Appendix B). For a sample Ebola Communication Pathways, also see Appendix D.
Coordination between levels is important in order to build partnerships and collaborate with organizations and institutions that operate at different levels, so the team can plan a comprehensive approach to SBCC for its audience.
Used correctly, SBCC should bolster the Ebola communication response and ultimately strengthen the health systems. In this case, we use the term “health systems” holistically to include individuals, households, and communities that produce health and demand health services, as well as those health facilities that serve and promote health and wellbeing.
There are a number of behavior change theories that provide stakeholders with guidance on developing programming for Ebola communication within a particular context. Information on the models is in Appendix E.
In risk communication, national and local government authorities need to provide information to the public in an understandable, timely, transparent and coordinated manner before, during and after a crisis. The objectives of risk communication are to enable people at risk to make informed decisions and actions in order to reduce the risk they face. Effective risk communications can instill and maintain the public’s trust in the local and national health system and convey realistic expectations about the health system’s capacity to respond and manage an outbreak. Risk communication also promotes effective exchange of information and opinion among scientists and public health experts during the alert phase, in order to better assess, manage, and coordinate preparedness and response activities. Another key element of risk communication is to detect and manage the spread of rumors and misinformation.
Every emergency, disaster or crisis evolves in phases. By understanding the pattern of the Ebola crisis, communication professionals can anticipate problems, predict and/or adapt to specific communication needs, and communicate more effectively during each phase. While this I-Kit will focus on preparedness, it is important to understand the stages of emergency communication, which include the following:
1. Pre-Crisis
Many disasters and crises can be anticipated. As such, it is critical to ensure that systems are in place beforehand, including a social mobilization and communication coordinating mechanism, an action plan and a call center. A foundational Ebola communication preparedness strategy can include basic messages that are tailored to the local context, communication protocols, available resources, and the roles and responsibilities of various actors. An important element of this phase is creating trust among all stakeholders.
2. Initial Phase
Once there is a confirmed Ebola outbreak, it is important to mobilize leaders, response staff and institutions to get information out quickly. Conducting mapping exercises and identifying trusted sources prior to such an event is crucial, because time is of the essence. Conducting rapid assessments continuously throughout the outbreak will help the team address the barriers that might spread the virus or contribute to a higher mortality count. Having accurate information and using credible and trusted spokespeople at this phase is key to minimizing confusion, rumors and misinformation. Spokespeople should be able to communicate scientific information and accurate facts in a way that is understandable to the general public.
3. Maintenance
As the crisis evolves and more information is known, social mobilizers/spokespeople should listen to stakeholders and pay attention to audience feedback, using that input to correct any rumors or misinformation. All public information communication plans should explain to social mobilizers/spokespeople the emergency recommendations and how to make decisions based on risks and benefits, in close consultation with the health authorities at the incident management system or other emergency response center.
4. Resolution
During this phase, it is important to ensure that community members do not become complacent. Communicators should reinforce messages through communication campaigns or other mechanisms so that audiences understand that a new and desired behavior is necessary to prevent future outbreaks.
5. Evaluation
This is the opportunity to carefully review how the communication strategy was implemented during the crisis; examine and record best practices, successes, challenges and lessons learned; and make changes as needed to more effectively address the issues if a similar crisis were to develop again. Gather lessons learned from all the partners and record these for future use.
For more detailed information on recommended actions within each of these stages, see Chapter 2: Ebola Communication Preparedness Stages and Guidance.
Accomplishing this may require policy changes as well as capacity strengthening for health communication managers and service providers. The table below shows the areas of capacity strengthening that will help to meet the needs of an Ebola outbreak communication campaign.
| Capacity Strengthening Areas for Ebola Preparedness Communication | |
| Vision, Leadership, and Governance | Ebola strategic communication preparedness emphasizes developing strategies, clarifying roles, managing competing demands and gaining commitments from stakeholders. Stakeholders can include communities, governments, international organizations, nongovernmental organizations (NGOs) and the private sector. Together, they will develop national Ebola communication preparedness strategies to prevent and contain Ebola. |
| Service Delivery | Ebola communication preparedness efforts usually include improving the skills of the service provider to enhance service delivery and quality assurance. Feedback loops need to be established between communities and health facilities with clear quality standards. In addition to standard technical training, health providers need to be well trained in interpersonal counseling and communication so that clients are motivated to practice safer Ebola behaviors. |
| Financing | For Ebola communication preparedness to gain traction, it is important to advocate for sustainable financing and develop mechanisms for financing through public/private partnerships and small grants using innovative communication approaches. |
| Human Resources | Capacity for Ebola communication preparedness should be built into the work force by engaging health care workers through training, incentives and, above all, motivation. |
| Health Information | An important part of Ebola communication preparedness is to ensure people use and share best practices and data to improve organizational communication and to make quick decisions during an emergency. Managing knowledge and information for managers, providers, clients and policy makers is critical. Everyone should have the latest information readily available to them. |
| Technology and Infrastructure | Ebola communication preparedness efforts should utilize innovative and appropriate technologies to reach out to managers, providers and clients. |
Back to Chapter 1