+ 123 456 7890
Health Belief Model
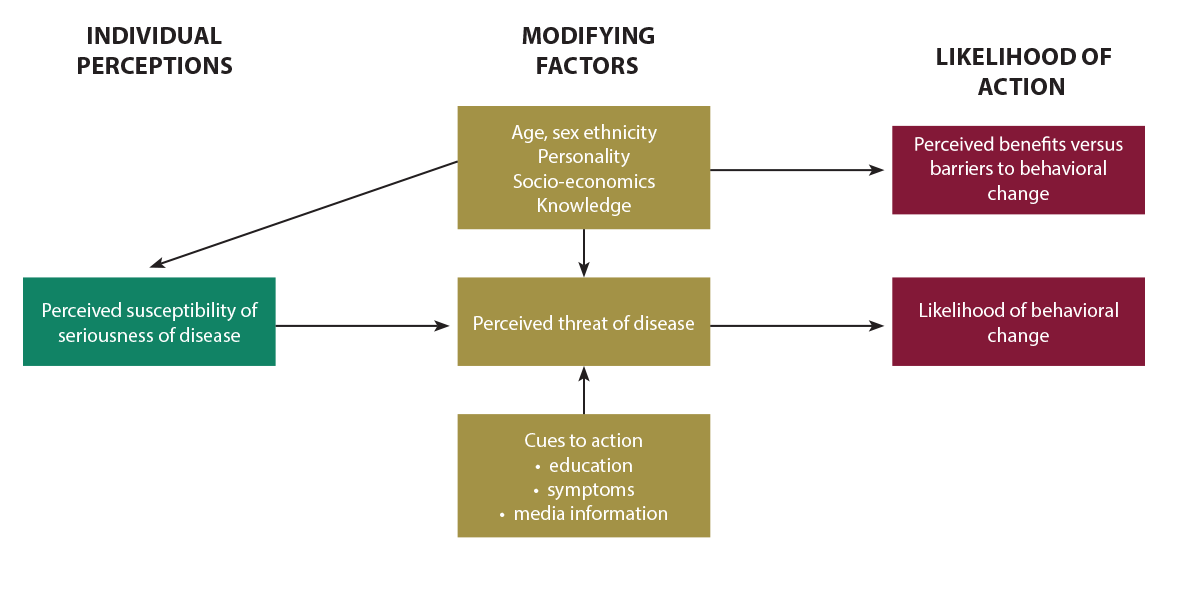 The Health Belief Model highlights how programs need to consider individual beliefs about the problem being addressed, and the costs and barriers associated with changing a behavior. According to the Health Belief Model, a person is likely to change behavior if he/she experiences:
The Health Belief Model highlights how programs need to consider individual beliefs about the problem being addressed, and the costs and barriers associated with changing a behavior. According to the Health Belief Model, a person is likely to change behavior if he/she experiences:
- Perceived Susceptibility/Seriousness: believing he/she is at risk.
For example, the mother believes she is at risk of buying SSFFC medicines or that her child will face severe consequences if treated with poor quality medicine.
- Perceived Benefits: believing that the behavior change will reduce risk.
For example, a mother believes that she is more likely to get good quality malaria medicine if she gets it from a government health facility, instead of the local drug vendor.
- Perceived Barriers: how one interprets the costs/barriers of the desired behavior.
For example, a mother is concerned about the time and transportation costs involved in going to the government health facility when her child is sick with fever, rather than simply buying malaria medicine from the local drug vendor.
- Cues to Action: strategies to activate “readiness.”
For example, a health provider recommends a quality medicine source when telling the mother her child tested positive for malaria.
- Self-Efficacy: feeling confident in one’s ability to take action.
For example, a mother feels that she is able to purchase malaria medicines from less risky, regulated sources.
How Can the Health Belief Model Be Applied?
The Health Belief Model is best used when promoting individual preventive behaviors, such as vendor or consumer purchasing or verification practices. It focuses on the beliefs and perceptions of the individual, so it is appropriate to change behaviors that are not heavily influenced by society and social norms. It tells us the importance of highlighting both the negative consequences of the current behavior and the positive consequences of alternative, suggested behavior.


