At this stage, you have identified your key barriers to FBP motivation, identified your intended audience(s), defined your objectives and the general strategic approach you plan to use.
This step pulls together resources, toolkits and guidelines that guide the development of SBCC approaches that will help address the identified barriers to FBP motivation. These can be adapted to your context and intended audience as you see fit.
The tools and resources have been organized around the five main categories of FBP motivation discussed previously:
- Self-Efficacy
- Status
- Social and Gender Norms
- Rewards
- Work Environment
Review your findings from your situation, root cause and audience analyses to remind yourself of the motivation barriers your FBP audience faces. Consider the approaches you have chosen to address those barriers. Then, read the relevant sections below and access the resources that will help you in designing your SBCC intervention.
Self-Efficacy
To improve FBPs’ levels of self-efficacy, SBCC interventions can design activities that address the four sources of self-efficacy:
- Mastery experiences. Provide opportunities for FBPs to successfully perform a task. Since success boosts self-efficacy, allowing providers to practice in a safe environment where success is more likely can be effective.
- Vicarious experience. Provide opportunities for FBPs to observe peers succeeding at a task. Having role models demonstrate success in performing a task can strengthen FBPs’ beliefs in their own ability to do the task.
- Verbal persuasion. Offer positive feedback and encouragement to FBPs for work done well. This can help FBPs confirm that they are performing well and that they are able to do what is expected.
- Emotional state. Create a positive work environment where stress and anxiety are reduced and positive feelings are heightened. Positive emotional stimulation can boost FBP performance.
Supervisors and facility management play a key role in providing relevant experiences, giving feedback, and influencing the FBPs’ environment. SBCC interventions seeking to impact self-efficacy may find it useful to place supervisors or management as the audience for the SBCC efforts. SBCC could be used to encourage management to implement any of the following activities or approaches:
- Deliberately create situations where FBPs can safely practice new skills or behavior change. These situations should be of moderate difficulty so that FBPs are challenged but still have good chances of success.
- Create behavior change strategies jointly with individual FBPs. These strategies should set specific, short-term goals that are reachable. FBPs can verbalize their plans and provide regular progress updates to supervisors.
- Learn about what interests individual FBPs and provide opportunities for them to pursue those interests.
- Create peer learning groups or provide opportunities for observing peers.
- Give FBPs autonomy in specific areas. Supervisors can identify certain areas where they feel comfortable giving FBPs autonomy to act and make their own choices.
- Provide specific praise and encouragement when FBPs perform well. The praise must be believable and consistent. Supervisors and management can also help FBPs understand their strengths and emphasize the importance of effort – rather than innate ability – in achieving tasks.
- Offer prompt, frequent, and specific feedback on tasks. Supervisors can provide specific methods for improvement the next time.
- Create a positive work environment where collaboration, encouragement, and honesty are emphasized.
There are also many non-supervisory SBCC methods for improving self-efficacy among FBPs. Some examples include:
- Using Entertainment Education (EE) approaches to model desirable behaviors. Whether through TV or radio soap operas, games, community theater, or music, EE presents relatable role models for FBPs. These role models overcome obstacles, adopt new behaviors, and successfully perform tasks in realistic ways, which can enhance FBPs’ feelings of self-efficacy.
- Using role-play activities to guide reflection and provide opportunities to practice skills. Forum Theatre uses a combination of observation and role play to help audiences see the familiar from a different perspective. Participants watch a performance, then analyze the performance and coach actors on new ways of constructing the narrative. This helps participants examine and reflect on the way things are being done. Rehearse for Reality allows participants to play themselves but with enhanced abilities and self-efficacy. Participants can practice new skills and see themselves succeeding.
- Using group discussion or learning groups paired with mass media to encourage reflection, discussion, and practice.
- Using trainings and job aids to build knowledge and skills. There are several training application approaches that can help bridge the knowledge-practice gap. One example is the Written Self-Guidance approach where FBPs write a motivational letter to themselves after the training. This self-affirming letter includes the training content that was most relevant to the FBP and encourages the FBP in attaining the goal.
The table to the right contains examples of programs and guidance for addressing self-efficacy among FBPs.
Perceived Place in Social Hierarchy/Status
Cultural power and status relationships typically stem from social norms as well as FBPs’ and clients’ perceptions of themselves and one another. Thus, tackling status-related challenges requires addressing deeply held values, beliefs, and attitudes – among FBPs and clients.
SBCC can create spaces for FBPs and clients to listen to each other, discuss and collaborate. Contact theory suggests that increased contact between groups can help reduce prejudice and conflict. However, effects are not as positive when the groups are of unequal status. In those cases, cooperative learning where members of different groups play essential roles in the process can increase empathy and positive feelings between groups. One strategy is to create opportunities for clients and FBPs to jointly work on projects that both groups view as important. Projects can use a variety of approaches and channels to create working and learning spaces, including community dialogue, mass media with listeners’ groups, community mobilization, and project-based learning.
The Puentes project in Peru brought communities and health workers together to create participatory videos that identified barriers to utilization of services. Together, they defined what quality services looked like and came up with an action plan for improvements. Health workers saw issues in a new way and were able to shift attitudes about the services they offered and the community they served.
SBCC can also influence perceptions on what is expected from FBPs and clients. SBCC activities can clearly communicate what is expected of FBPs through support supervision meetings, print reminders on clinic walls or in job aids, trainings, TV or radio ads and programs, coaching, or community theatre. These materials and activities can emphasize the expectation of respectful, non-discriminatory treatment.
Clients can also be sensitized to their role in the client-provider partnership and be encouraged to be an informed client that provides relevant information and asks key questions.
The Smart Patient initiative in Indonesia used client coaching to improve the client-provider interaction. Clients received 20 minutes of coaching on their rights, and how to ask questions, express concerns, and ask for clarification. Client educators would assess clients’ needs and skills, seek to understand client motivation, prepare questions and rehearse with the client, and then clients would take action with a provider. Both providers and clients responded positively, and client participation increased.
Both clients and FBPs need positive role models in adopting new beliefs and attitudes. Entertainment Education can be an effective way of presenting role models who demonstrate positive attitudes and behaviors (like trusting health workers, using services, or speaking with respect to clients regardless of status) and change just like the audience needs to.
The Nepal Radio Communication Project implemented two radio serial dramas to address issues of caste, status, and trust in providers. One soap opera, designed for the general public, sought (among other things) to improve perceptions of health workers and to model men and women actively seeking better health conditions. A distance education radio serial for health workers told the story of two health workers who modeled a client-oriented approach, desirable attitudes and behaviors, and strong technical knowledge. Health workers received supporting discussion guides and pre-stamped feedback letters. The program also used radio spots based on the serial dramas, trainings, and print materials to support behavior change.
Changing status-related beliefs and attitudes also requires self-reflection. SBCC can take advantage of values assessments used in facility training or support supervision, reflection journals used with TV/radio serials, or job aids that encourage time to reflect before taking action. It is also important to examine FBPs’ workloads, stressors, and contextual factors. Sometimes FBPs treat certain populations poorly as a way to cope with difficulties at work. Helping FBPs obtain and practice effective coping skills can ease status-related tensions.
The table to the right contains examples of programs and guidance for addressing status among FBPs.
Social and Gender Norms
There are many social and gender norms that influence how FBPs interact with their clients. You likely uncovered some of those norms through the Situation Analysis. However you may need to do additional research to understand what local norms are barriers to quality service provision (both among FBPs and clients) and the underlying reasons why they exist. This can be done through key informant interviews, focus group discussions or interactive research techniques.
In Egypt, there were strong norms for conception immediately after marriage. Providers did not feel they could advise their clients to wait to have children because of the strong community norms. Even when they believed it would be best for the family, they did not actively encourage the behavior out of fear of ridicule, rejection, and losing clients’ trust.
Once you understand what social and gender norms need to be addressed, you can design focused interventions. Normative change typically requires dialogue – between partners, families and communities. This is especially true when community members incorrectly perceive that their attitudes and behaviors differ from other community members’ (pluralistic ignorance). In these cases, a large group of individuals reject a norm privately but participate in it because they believe others support it. Open, honest dialogue about the norm can help community members realize that others do not support the norm and desire change. Even in situations where pluralistic ignorance does not exist, FBPs and community members need to confront their values and openly discuss the impact of those values on their community and the health system. SBCC approaches to encourage this type of discussion include community dialogue, TV/radio listeners’ groups, community mobilization, and peer-to-peer approaches.
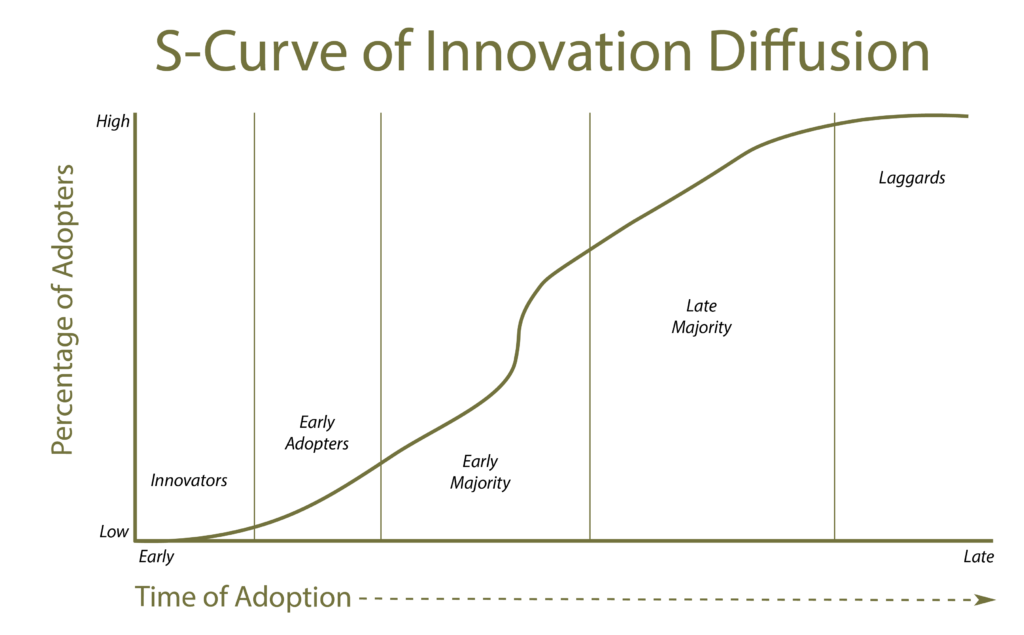
Social change also requires early adopters that others who are considering change can look to – both in the community and at the health center (see graphic below). SBCC projects can identify FBPs and community members who are already practicing supportive norms or ones who might be willing to make a change (innovators or early adopters). Then, a number of approaches can be used to spread that norm, including positive deviance and peer networks; testimonials on radio, print, or web; or norm champions. Mass media can help create a sense that a certain behavior or attitude is normative, and Entertainment Education can effectively use modeling to show how change could occur.
Adapted from Pinkett
In designing programs for FBPs that will target gender-related norms, consult the Gender Equality Continuum as a means of evaluating whether your program contributes to gender equity.
The table to the right contains examples of programs and guidance for addressing social and gender norms among FBPs and community members.
Rewards
Projects can use SBCC to help FBPs feel rewarded for their work. Advocacy efforts aimed at facility managers and ministry staff can be used to encourage financial rewards and other systemic changes that providers view as rewarding. For example, advocacy campaigns can urge ministry officials to provide more opportunities for learning and training or to create systems for merit-based advancement. It can also encourage local control of incentives to enable facility managers to be creative with rewards. Once rewards systems are in place, SBCC can be used to advertise those rewards and encourage FBP participation through mass media, social and peer networks.
SBCC can be used to recognize FBP contributions and to show appreciation. These recognition campaigns can be done at the facility-level where supervisors and peers recognize efforts and good work. Or they can be done at the general public level where community members or ministries express appreciation for the FBPs. A variety of channels can be used to recognize providers, including TV or radio spots, community events, print materials in clinics, Facebook or WhatsApp groups, closed-network SMS groups, ministry events, or websites.
PSI designed an incentive program to recognize and reward Most Improved and High Performing providers. The program tracked provider performance and improvement related to provision of services and program goals. Motivation among providers increased when improvement was recognized.
Helping FBPs see and believe the importance of their work can also improve motivation and performance. SBCC can be used to design data visualizations that show the impact of FBPs’ work, community dramas or TV/radio serials that show the value of FBPs’ efforts, or client testimonials that demonstrate how FBPs helped them.
The Women’s Health Project helped providers see the benefit of providing IUDs and the ways it could improve clients’ lives by producing a cost/time analysis to the providers in their clinics.
The table below summarizes financial and non-financial incentives that can be used to reward FBPs. While SBCC programs do not usually directly provide financial incentives, they can advocate for financial rewards.
| Direct Incentives* | |
|---|---|
| Financial Incentives | Non-Financial Incentives |
| Terms and conditions of employment: salary/stipend, promotion, pension, insurance, allowances and leave | Job satisfaction/work environment: autonomy, role clarity, supportive/facilitative supervision and manageable workload |
| Performance payments: performance-linked bonuses or incentives | Preferential access to services: health care, housing and education |
| Other financial support: fellowships, loans and ad hoc | Professional development: continued training, effective supervision, study leave, career path that enables promotion and moving into new roles |
| Formal recognition: by colleagues, health system, community and wider society | |
| Informal recognition: T-shirts, name tags, and access to supplies/equipment |
| Indirect Incentives* | |
|---|---|
| Health System | Community Level |
| Well-functioning health systems: effective management, consistent M&E, prompt monthly payments, safe environment, adequate supplies and working equipment | FBPs witnessing visible improvements in health of clients |
| Sustainable health systems: sustainable financing, job security | Peer organizations that support FBPs |
| Responsive health systems: trust, transparency, fairness and consistency |
Work Environment
Interventions to improve FBPs’ work environment should start with an assessment to understand the work environment, what FBPs need, and what could be done to improve the climate. You may have discovered some of this information during the Situation Analysis. However, you will likely need to do some more research to understand the work environment. This can be done by talking to both clients and FBPs.
Workplace environment interventions require normative change – at the organizational, managerial, and individual provider levels. SBCC interventions need to address the values, assumptions, behavioral norms, and symbols that impact how FBPs interact with each other and clients.
Health facility management plays a key role in creating a positive work environment with norms for teamwork, recognition, civil treatment of clients, equal participation, social sensitivity, and quality work. Managers also need skills in effective management and supervision, leadership, setting a vision, and creating efficient systems. Thus, health facility managers are often a primary audience for SBCC efforts.
Given management’s role in the facility, many SBCC interventions to improve the work environment include leadership training. These trainings are aimed at helping facility leadership to set and communicate a strong vision, practice supportive supervision and effective management, improve management systems, and recognize staff accomplishments. Some strategies include:
- Education and coaching
- Action-learning workshops
- Leadership learning modules
- Simulations and role playing
- Reflective and visionary practice
FBPs are also a key SBCC audience for workplace environment interventions. Norms need to change across the health facility - not just at leadership levels - and interventions that do not involve employees are rarely successful. Many successful SBCC interventions use FBP change champions supported by leadership and a clear vision for improvement. These change champions help lead the cause in setting and practicing new norms and behaviors, including praising and recognizing colleagues, interacting positively with clients, supporting colleagues emotionally, sharing responsibilities, and promoting teamwork.
Some health facilities have implemented civility interventions to encourage FBPs to treat all people in the workplace civilly and respectfully. These interventions also aim to increase collaboration, teamwork, and engagement through facilitated discussions, role-playing and action plans. Print reminders, civil role models, and closed-network SMS encouragements can support the core activities.
The Civility, Respect, and Engagement at the Workplace (CREW) intervention has been used to increase civil and respectful interactions in health facilities. CREW raises awareness about the importance of civility and helps staff develop a shared understanding of how civility can help them achieve work goals. Trained facilitators meet frequently with specific work groups and facilitate discussions that define civil behaviors and aim to change behaviors, attitudes, and emotions. Facilitators use role-plays and action plans to encourage problem solving and group interaction. Using CREW has helped improve the work environment significantly by increasing civility, trust, respect, and empowerment.
SBCC can also be used to improve teamwork at the facility. These interventions focus on improving teambuilding, group communication, conflict management, and a sense of collaboration. Teamwork interventions often involve teamwork training, problem-based learning teams, simulations, feedback sessions, joint redesign of work practices, change teams, communication shortcuts with mnemonic devices, and informal conversations. Some of the SBCC tools used in teamwork interventions include:
- Podcasts
- Bulletins and emails
- Self-review and communication
- Facilitator debriefs
- Checklists
In Bolivia, the Curamericas/CSRA team improved child survival by brining partners and communities together. The team held mortality analysis workshops where staff thoroughly investigated mortality cases, identified the barriers to health care, and then developed plans to navigate around those barriers in the future. As a result, health staff and the community took positive and effective action to improve child survival.
The table to the right contains examples of programs and guidance for improving the work environment.


No Comments