There is no single SBCC technique or communication channel that is known to improve provider behaviors. Depending on the identified performance gap, supportive supervision can be used to help providers adopt and maintain new behaviors and stay motivated to do their jobs well.
Many service delivery programs already regularly provide supportive supervision through training follow-up and routine monitoring. Very often, however, routine supervision focuses on improving the provider’s clinical data collection, reporting, or appearance and organization. A provider behavior change approach to supportive supervision focuses not only on training and improving skills, but also on the specific barriers a provider faces in adopting a new behavior. A provider behavior change approach to supportive supervision uses insights gathered during the audience analysis to develop strategies for maintaining long-term behavior change, framed around what the provider needs and values.
In addition to training, a supportive supervision plan may include:
- Monitoring and management through a supervisor
- New job aids and tools, which may use multiple media platforms (such as SMS, mobile phones, and short videos) to support better counseling and include support to use them properly
- Coaching and routine support provided by a supervisor and framed around a specific performance improvement plan
- Technical support through hotlines or videos
- Mentoring support provided by a high-performing peer or manager
An Example: Applying a Provider Based Framework
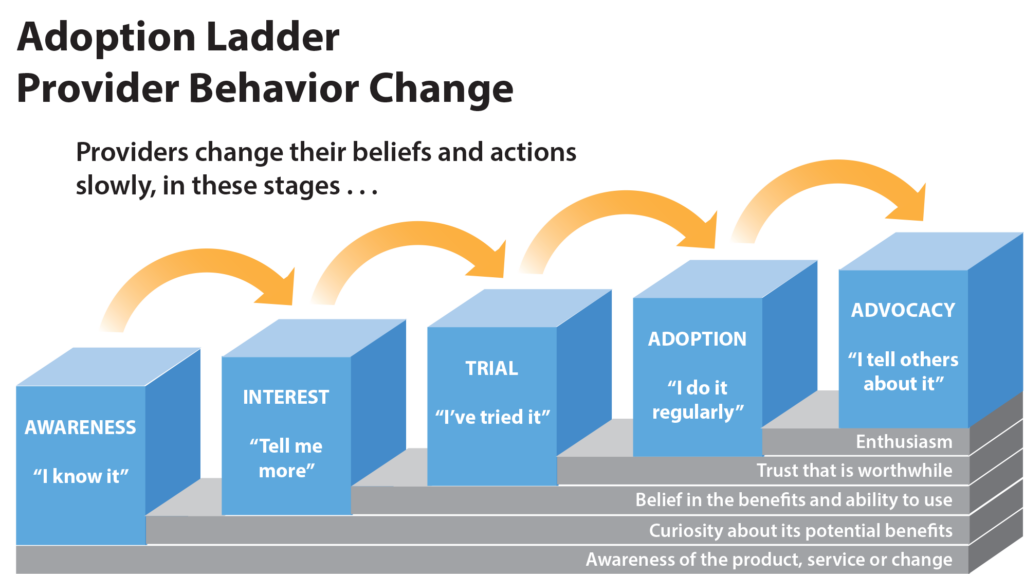
PSI developed and implements a system for provider behavior change in its social franchise clinics based on the Stages of Change (Transtheoretical Model). PSI uses the process to address gaps in a wide range of provider behaviors and health areas. The process recognizes that providers are at varying stages of behavior adoption:
- Awareness – The provider knows about the targeted behavior.
- Interest – The provider has expressed interest in adopting new behavior.
- Trial – The provider has taken an initial step to try the new behavior.
- Adoption – The provider has adopted the new behavior and regularly uses it
- Advocacy – The provider is encouraging others to adopt the new behavior because it has helped the provider achieve specific needs, such as more clients, more revenue, or more efficient work.
Another way of supporting providers in their new behaviors is the medical detailer approach. Medical detailers – who have fewer qualifications than supervisors – can pay visits to providers to help improve service availability and quality. The medical detailers discuss services with providers and uncover barriers that may prevent them from offering or improving services. If the medical detailer finds that the provider has training but lacks confidence in a certain skill, for example, the program can plan on-the-job training and supervision during special service days. If the medical detailer finds that the provider wants to serve youth but faces opposition by parents and community leaders, the program can plan SBCC activities to constructively engage those gatekeepers and influencers.
Interventions to change a provider’s behavior must first identify where a provider is in the Stages of Change and identify the main barriers that prevent the provider from moving to the next stage.
The process of identifying and developing tailored interventions to address the gaps in provider behavior follows four primary steps:
- Planning – Similar to the audience analysis, identify targeted providers and prioritize provider segments. Examples of segments include providers working in urban areas, providers delivering services at high- or low-volume facilities, and providers offering integrated services.
- Audience analysis to uncover provider needs – Using data gathered through methods like provider observation, client feedback, review of routine recordkeeping practices, client exit interviews, and mystery clients visits, develop provider profiles that describe the prioritized providers’ current performance, barriers to adopting new behaviors (knowledge, skills, motivation, etc.), key values, and expectations.
- Development of a tailored behavior solution to address the performance gaps and behavioral barriers. Develop communication tools tailored to address the identified gaps. The tools could include a range of materials to address skills barriers (training or better job aids, motivation barriers) or support coaching and mentoring tools and strategies.
- Reinforce the value of the solution – The fourth component is an ongoing process to remind providers how the behavior has benefited them and their clients. Reinforcement occurs through routine support supervision visits, regular acknowledgment and rewards, and/or recognition through community events, clinic “provider of the month” communications, and other methods to help sustain motivation and prevent providers from going back to their old habits.
 Example: WhatsApp
Example: WhatsApp
To strengthen supervisory support for Community Health Workers (CHWs) in 2 areas in Kenya, a mobile learning intervention launched a WhatsApp group for CHWs and their supervisors. The WhatsApp group enabled the group to engage in multiple forms of supervision: peer-to-peer, group, and one-on-one. The vast majority (88%) of the communication happening in the group related to predefined supervision objectives. The WhatsApp interactions helped supervisors understand the situation on the ground and ensure quality. It also helped users share relevant information with one another and create a supportive environment. Read more here.